MYOCARDIUM AR ATLAS
Interactive 3D Version Available
Explore this anatomy in full 360° rotation with our interactive 3D viewer
View in 3D →MYOCARDIUM
The myocardium is the thick, muscular layer of the heart wall responsible for the contractile function that pumps blood throughout the body. Composed primarily of cardiac muscle cells, it varies in thickness in different chambers of the heart, being thinner in the atria and significantly thicker in the ventricles. This difference reflects the varying demands placed on each chamber; the ventricles, especially the left ventricle, require more force to propel blood into the systemic circulation. The left ventricle's myocardium is notably thicker than that of the right ventricle, as it must generate higher pressure to distribute blood to the entire body.
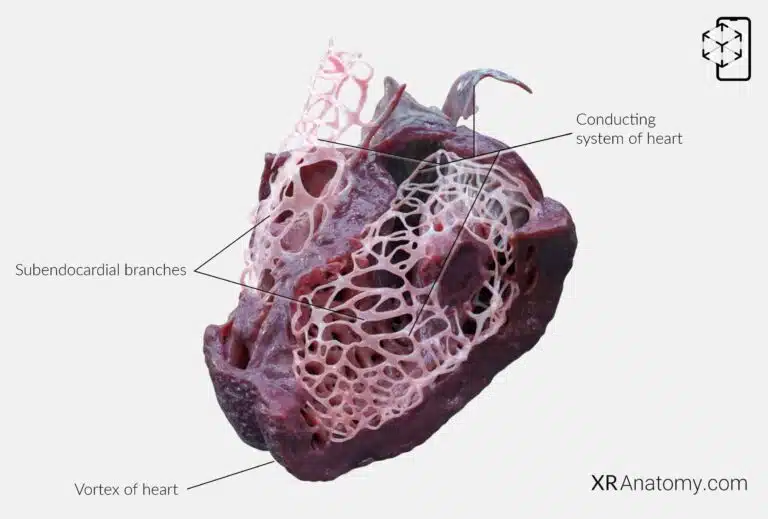
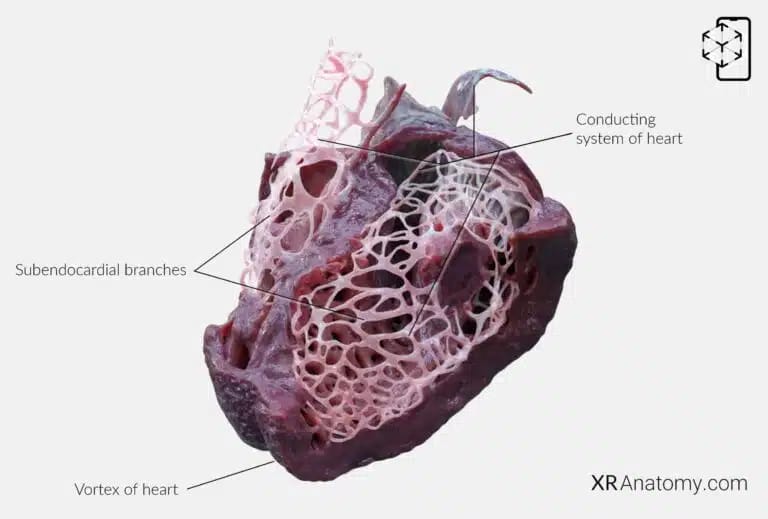
At the heart's apex, where the two ventricles meet, the muscle fibers of the myocardium twist and spiral to form the vortex of the heart. This arrangement allows for an efficient motion during contraction.
Embedded within the myocardium is the conducting system of the heart, a specialized network of cells that generate and transmit electrical impulses. This system ensures the coordinated contraction of the heart muscle, regulating the heartbeat and maintaining proper rhythm. It includes structures such as the sinoatrial node, atrioventricular node, and the bundle branches, which work together to synchronize the cardiac cycle.
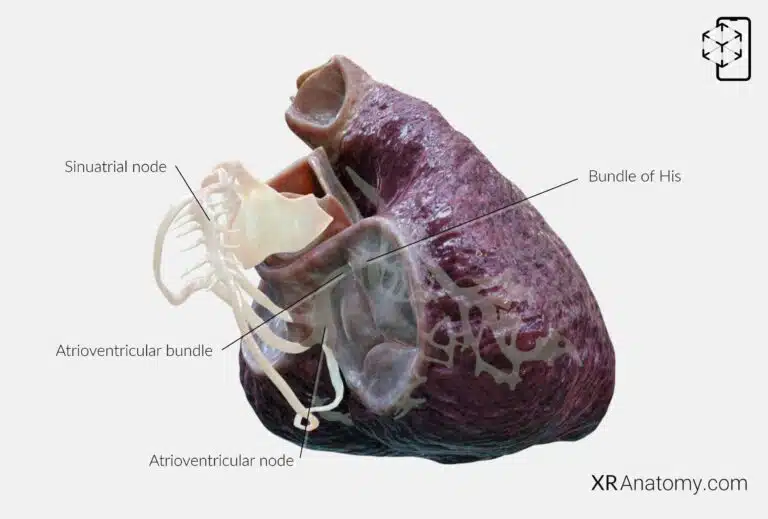
CONDUCTING SYSTEM OF ATRIA
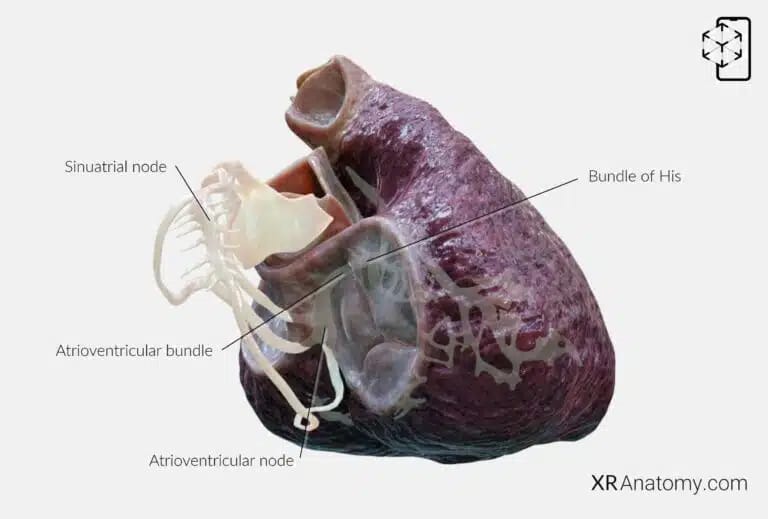
At the core of this conducting system, is the sinoatrial (SA) node, often referred to as the natural pacemaker of the heart. Shaped somewhat like a tadpole, the SA node is located in the right atrium near the opening of the superior vena cava, within the terminal groove. It generates electrical impulses that spread firstly throughout the atria.
The electrical impulse then reaches the atrioventricular (AV) node, a specialized cluster of cells situated in the right atrium near the septum, in an area known as the Triangle of Koch. The AV node acts as a critical gateway, briefly delaying the impulse before transmitting it to the ventricles. This delay ensures that the atria have enough time to fully contract and empty their blood into the ventricles before ventricular contraction begins.
From the AV node, the impulse travels down the atrioventricular bundle, also known as the Bundle of His. This bundle of specialized fibers penetrates the fibrous skeleton of the heart, allowing the electrical signal to pass from the atria to the ventricles. It serves as the only electrical connection between these chambers, ensuring synchronized contraction and efficient pumping action.
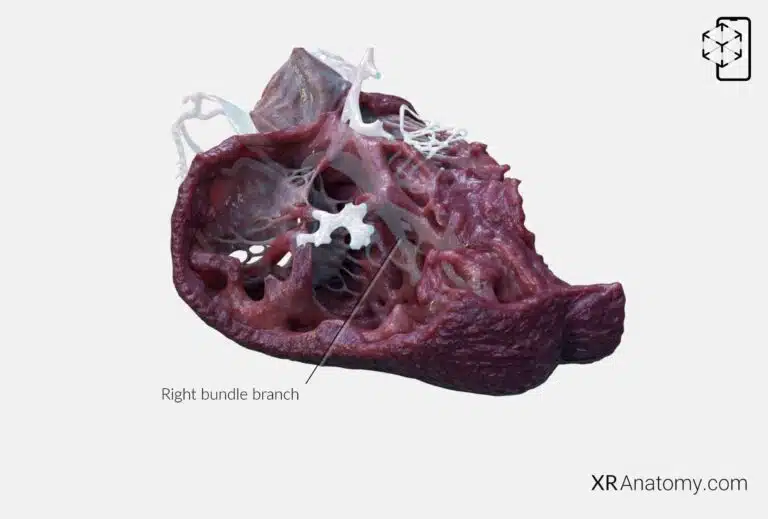
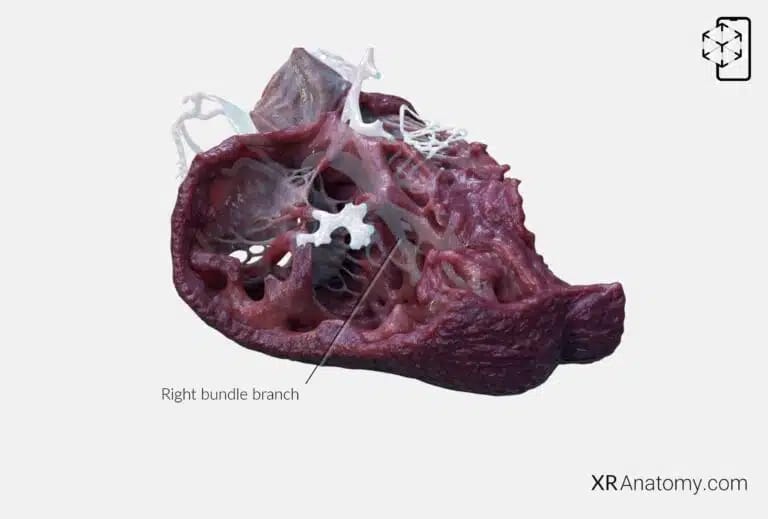
RIGHT BUNDLE BRANCH
The atrioventricular bundle divides into two main pathways: the right bundle branch (RBB) and the left bundle branch. The RBB specifically carries electrical impulses along the right side of the interventricular septum, beneath the endocardium, toward the right ventricle. As it progresses, it reaches the moderator band—a muscular band crossing the ventricular cavity. From there, it branches extensively in the myocardium of the right ventricle.
In parallel, the left bundle branch travels beneath the endocardium on the left side of the septum, extending toward the left ventricle. It divides into smaller branches that distribute the electrical impulse throughout the left ventricular myocardium.
This arrangement allows both ventricles to contract simultaneously, promoting efficient blood ejection into the pulmonary artery and aorta. The precise conduction through these bundle branches is essential for maintaining the heart's rhythm and synchrony.
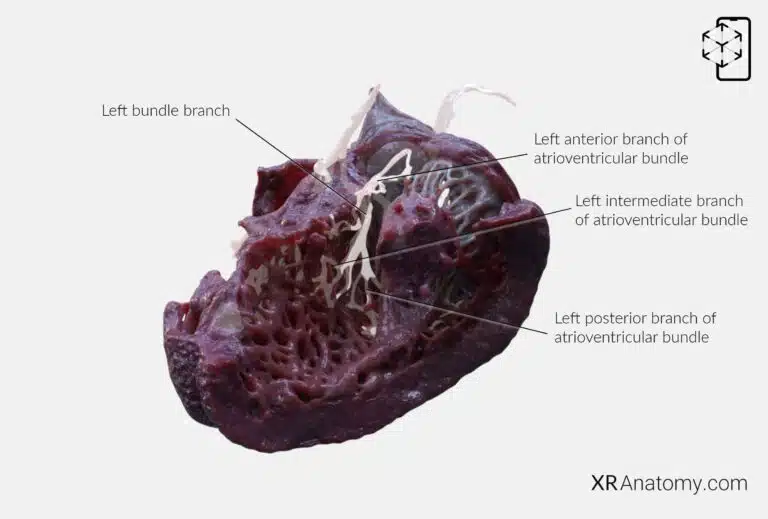
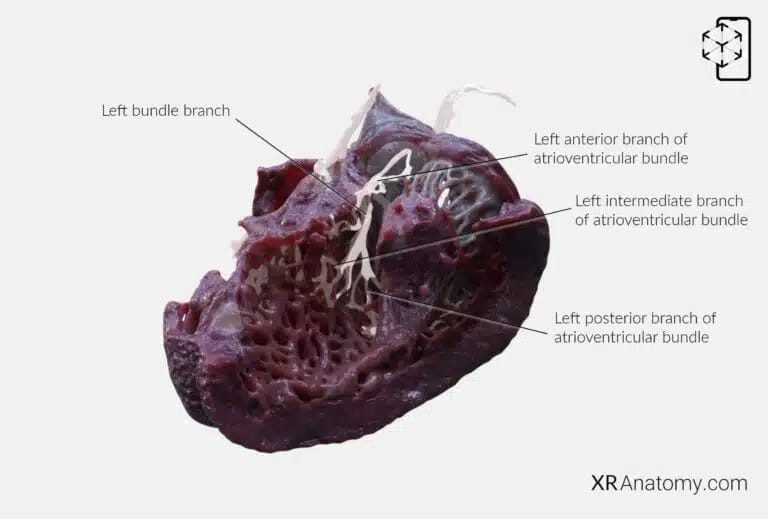
LEFT BUNDLE BRANCH
The left bundle branch further divides into three main fascicles to ensure comprehensive distribution of the electrical impulse within the left ventricle. The left anterior branch of the atrioventricular bundle courses along the superior aspect of the left ventricle toward the anterolateral papillary muscle. It spreads over this muscle in multiple directions, facilitating a uniform contraction of the anterior wall.
The left intermediate branch runs superficially through the subendocardium along the septum toward the apex of the left ventricle. This branch ensures that the interventricular septum and the apex receive synchronised electrical stimulation, contributing to the effective pumping action of the heart.
The left posterior branch travels along the inferior aspect of the left ventricle toward the posteromedial papillary muscle. It disperses across this muscle, synchronising the contraction of the posterior wall of the left ventricle.
These branches end in subendocardial branches, also known as Purkinje fibers. These specialized fibers form an extensive network lining the inner ventricular walls, penetrating the myocardium. They interface directly with cardiac muscle cells, ensuring rapid and synchronized transmission of the electrical impulse throughout the ventricles, leading to a coordinated and forceful contraction.
The integrity of this conduction system is vital for maintaining the heart's rhythm and efficiency. Disruptions can lead to arrhythmias or conduction blocks, affecting cardiac output and overall cardiovascular health.
BIBLIOGRAPHY
1. Gray H, Lewis W. Angiology. In: Anatomy of the Human Body. 1918. p. 526–542.
2. Gosling JA, Harris PF, Humpherson JR, Whitmore I, Willan PLT. Human anatomy: color atlas and textbook. 6th ed. 2017. 45–58 p.
3. Anderson RH, Spicer DE, Hlavacek AM, Cook AC, Backer CL. (2013). Anatomy of the cardiac chambers. In Wilcox’s Surgical Anatomy of the Heart (4th ed., pp. 13–50). Cambridge University Press.
4. Fritsch H, Kuehnel W. Color Atlas of Human Anatomy. Vol. Volume 2, Color Atlas and Textbook of Human Anatomy. 2005. 10–42 p.
5. Moore K, Dalley A, Agur A. Clinically Oriented Anatomy. Vol. 7ed, Clinically Oriented Anatomy. 2014. 132–151 p.
6. Ho SYen. Anatomy for Cardiac Electrophysiologists: A Practical Handbook. Cardiotext Pub; 2012. 5–27 p.
7. Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. London: Elsevier; 2016.
8. Moore KL, Agur AMR, Dalley AF. Essential Clinical Anatomy. 5th ed. Philadelphia: Wolters Kluwer; 2015.