RIGHT ATRIOVENTRICULAR VALVE AR ATLAS
Interactive 3D Version Available
Explore this anatomy in full 360° rotation with our interactive 3D viewer
View in 3D →TABLE OF CONTENTS
RIGHT ATRIOVENTRICULAR VALVE
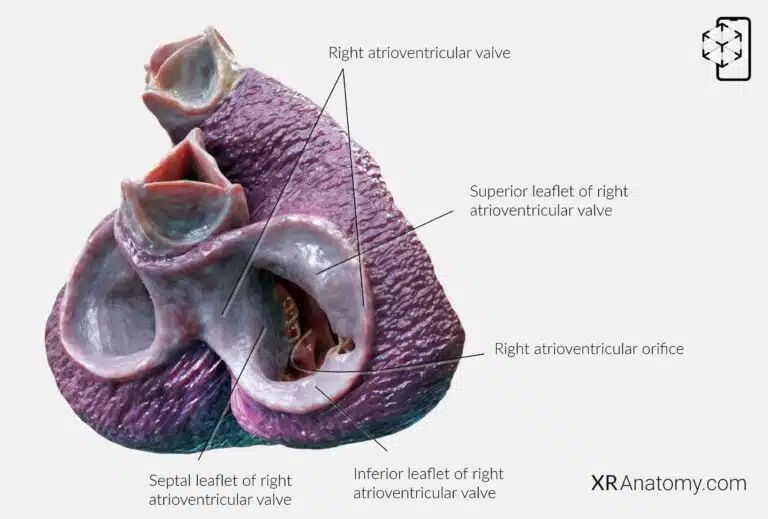
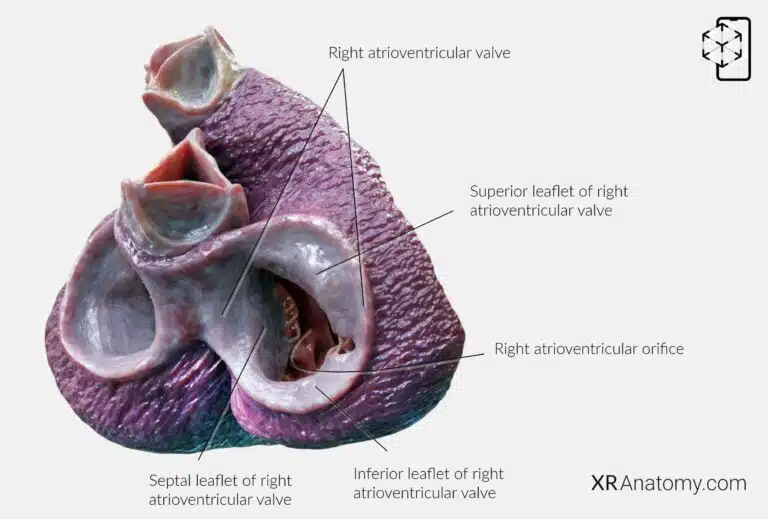
The right atrioventricular valve, commonly known as the tricuspid valve, is a critical component of the heart's valvular system. It is one of the two atrioventricular (AV) valves and functions to regulate blood flow between the right atrium and the right ventricle. By opening and closing during the cardiac cycle, it ensures unidirectional blood flow and prevents backflow into the atrium when the ventricle contracts. The tricuspid valve is characterized by its three leaflets or cusps: the anterior, posterior, and septal leaflets.
The superior (anterior) leaflet is the largest and is situated at the top of the valve structure.
The inferior (posterior) leaflet is located at the bottom, playing a vital role in sealing the orifice during ventricular contraction.
The septal leaflet, positioned adjacent to the interventricular septum, is unique due to its numerous tendinous cords that connect directly to the ventricular septum. This leaflet's hinge is inserted closer to the apex of the heart compared to the hinge of the mitral valve's leaflets on the left side.
The valve surrounds the right atrioventricular orifice, the opening between the right atrium and right ventricle. Notably, this orifice is larger than the left atrioventricular opening, accommodating the volume of blood returning from the body.
A crucial aspect of the tricuspid valve's function is the presence of a tension apparatus consisting of papillary muscles and chordae tendineae. This apparatus prevents the valve leaflets from inverting or prolapsing into the atrium during ventricular systole (contraction). The papillary muscles contract simultaneously with the ventricular myocardium, tightening the chordae tendineae and securing the leaflets in place. This coordinated action ensures efficient closure of the valve.
BIBLIOGRAPHY
1. Gray H, Lewis W. Angiology. In: Anatomy of the Human Body. 1918. p. 526–542.
2. Gosling JA, Harris PF, Humpherson JR, Whitmore I, Willan PLT. Human anatomy: color atlas and textbook. 6th ed. 2017. 45–58 p.
3. Anderson RH, Spicer DE, Hlavacek AM, Cook AC, Backer CL. (2013). Anatomy of the cardiac chambers. In Wilcox’s Surgical Anatomy of the Heart (4th ed., pp. 13–50). Cambridge University Press.
4. Fritsch H, Kuehnel W. Color Atlas of Human Anatomy. Vol. Volume 2, Color Atlas and Textbook of Human Anatomy. 2005. 10–42 p.
5. Moore K, Dalley A, Agur A. Clinically Oriented Anatomy. Vol. 7ed, Clinically Oriented Anatomy. 2014. 132–151 p.
6. Ho SYen. Anatomy for Cardiac Electrophysiologists: A Practical Handbook. Cardiotext Pub; 2012. 5–27 p.
7. Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. London: Elsevier; 2016.
8. Moore KL, Agur AMR, Dalley AF. Essential Clinical Anatomy. 5th ed. Philadelphia: Wolters Kluwer; 2015.